What are my treatment options for chronic hemorrhoids?
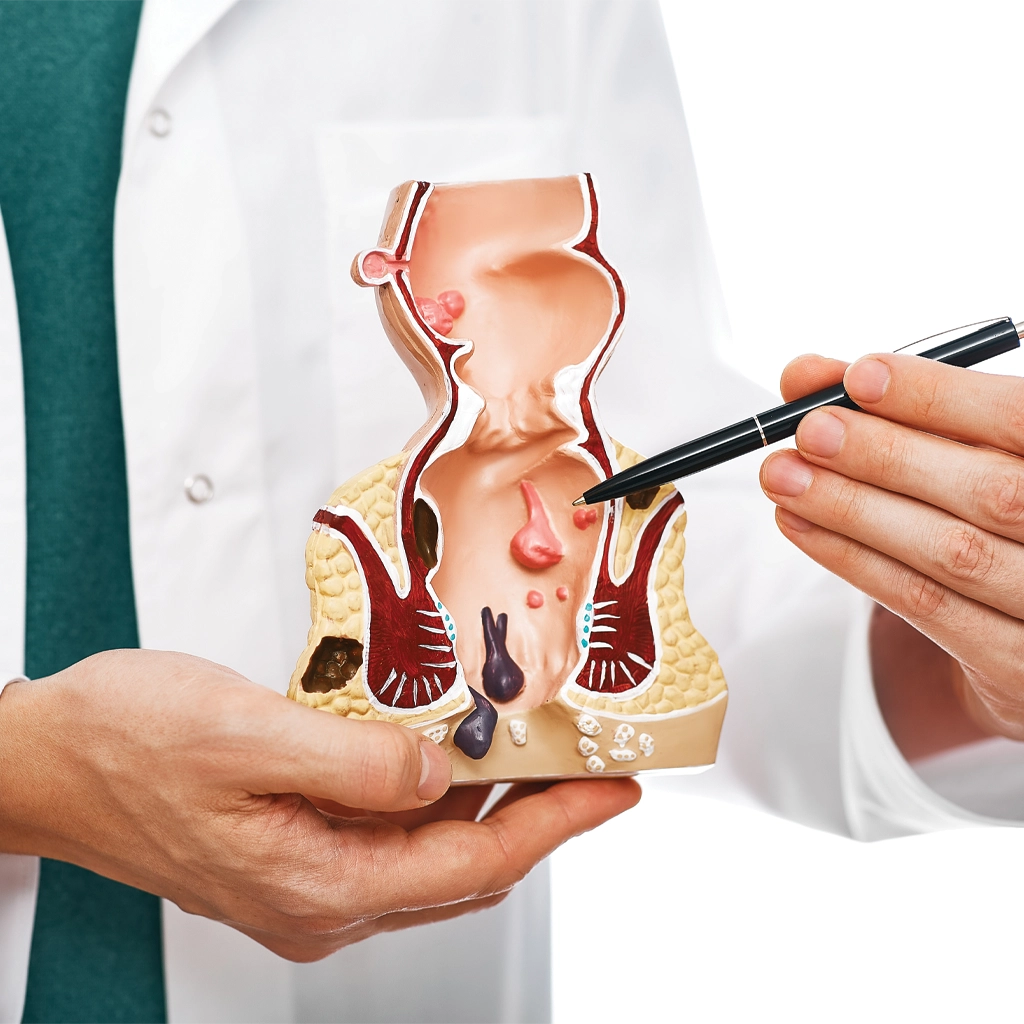
At first, physicians recommend treating hemorrhoids with conservative methods, such as diet changes, topical creams, sitz baths and pain relievers. If the symptoms persist and do not respond to conservative treatment, and the hemorrhoids are internal (meaning they remain inside the body) there are several approaches to treat them.
Hemorrhoidectomy is a surgery to remove chronic hemorrhoids. Unfortunately, surgery carries risks and potential complications that can include infection, bleeding, rectal prolapse and more. Recovery can be more difficult than other types of surgery because regular bowel movements can put pressure on the surgical site, causing pain. Although it is effective, this surgery is associated with intense postoperative pain and a prolonged time to return to normal activities.1,2
A less invasive treatment called Rubber Band Ligation is sometimes recommended to treat hemorrhoids. This involves wrapping a small rubber band around the base of a hemorrhoid, which cuts off blood, causing it to shrink and fall off within a few days. However, this approach is also associated with pain and complications, especially for those taking antiplatelet or anticoagulant medication, who have a higher risk of hemorrhage and infectious complications.3
A new and minimally invasive option offered by the doctors at VISA is called Hemorrhoidal Artery Embolization or HAE. It is safe and effective4, and achieves similar outcomes to surgery but with far less pain5 and a much shorter recovery.
You can learn more about the HAE procedure by clicking here »